70% of e-health projects fail before going to market
Between 60% and 80% of digital projects fail. In e-health, the figure is even worse: 70%.
After evaluating more than 30 projects for France 2030 and Bpifrance, the conclusion is implacable: only 3 out of 10 make it through to operational deployment.
But why? It’s never the technology. It’s always the organization.
The three pitfalls that kill projects
A start-up develops a promising algorithm over 18 months.
3 months to launch: discovery that medical device classification requires a further 24 months’ clinical study. Budget exhausted. Project abandoned.
A brilliant technical solution is designed without consulting end-users.
The result? Virtually zero adoption. Caregivers find the interface unsuited to their daily workflow.
A telemedicine tool is built without cybersecurity analysis.
First HDS audit: 47 critical non-conformities. Complete overhaul necessary.
What do they have in common? The absence of a structured methodology that simultaneously integrates technical, regulatory, human and business aspects.
Where the JuliaShift method comes from
My approach combines three rarely connected universes:
17 years with the French Army Health Service: structuring projects in constrained environments where error is not an option. In an overseas operation, when your telemedicine system has to operate at 45°C with an unstable satellite connection, you develop an obsession with resilience.
Scale-up HealthTech: expansion director, I deployed e-health solutions in 12 European countries. I’ ve experienced the pitfalls: multi-country compliance, cultural adaptation, organizational complexity.
France 2030 expert: as an evaluator for Bpifrance, I have developed a precise reading grid of success/failure factors. Unique observatory position on what really works.
Hybridization: military rigor (risk management) + Lean Startup (rapid field validation) + generative AI (prototyping acceleration). This alignment reconciles agility and compliance, speed and security.
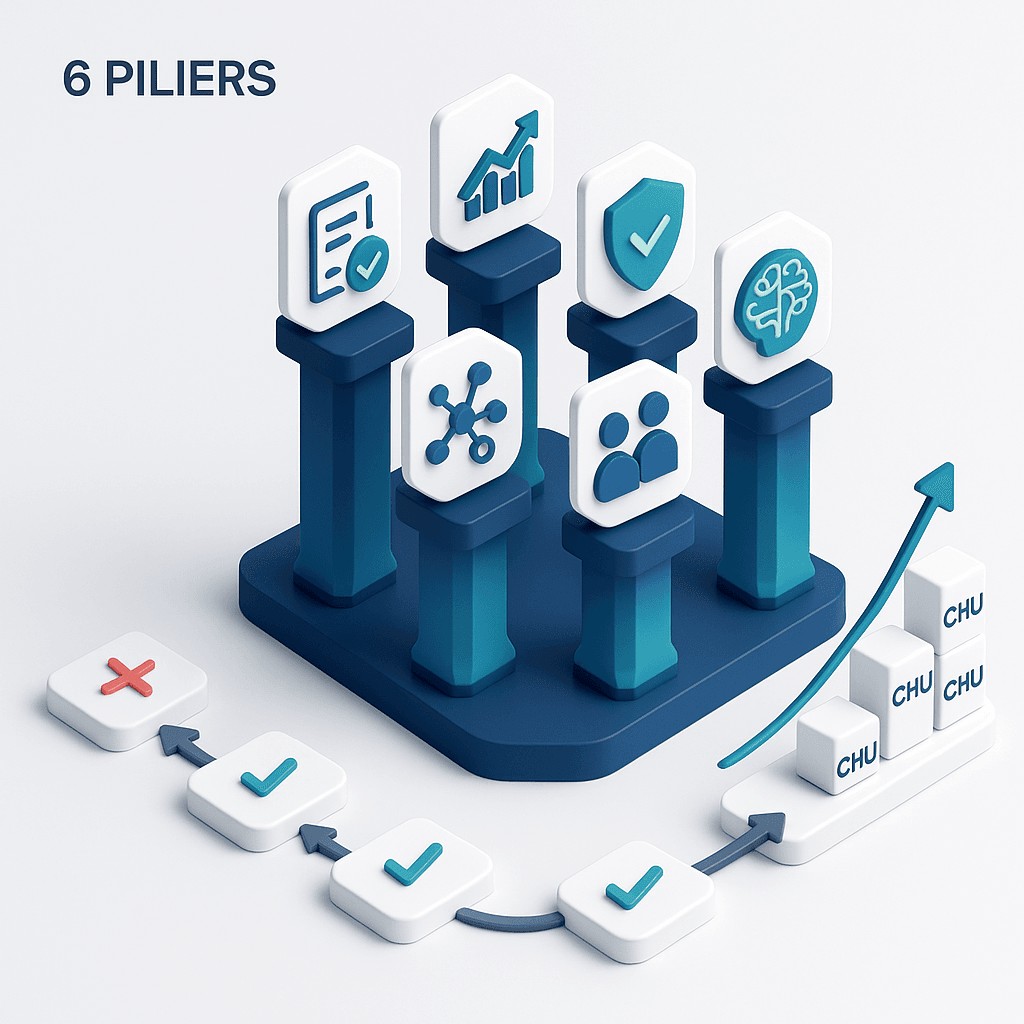
The 6 pillars of structuring
Pillar 1: Regulatory expertise from Day 1
The pitfall: Develop for 18 months, then discover the regulatory constraints.
The approach: Regulatory integration from D1, with adaptive roadmap.
Why? The healthcare sector is the most regulated in the world. MDR/IVDR, RGPDHDS, NIS2 cybersecurity… Each regulation impacts technical architecture and timeline.
What we do differently:
- Regulatory classification diagnosis week 1
- Compliance roadmap synchronized with product roadmap (no document big bang on D-30)
- Anticipation of clinical studies from the design phase
Pillar 2: Strategic health go-to-market
The trap: “Our product is great, it will sell itself.”
The approach: market validation before line of code, sales strategy adapted to healthcare sales cycles (18-36 months).
Why is this so? The healthcare market is not a classic B2B market. Multiple decision-makers (management, CIOs, doctors, IMGs) with conflicting objectives. Rigid budgets. Standardized purchasing processes.
Customer case: Startup bed management tool. Targeted CIOs (buyers). But real prescribers = healthcare executives (users). Pivot: 0 → 12 CHU customers in 18 months.
Pillar 3: Data security and compliance
The catch: “We’ll deal with cybersecurity later.”
The approach: Security by design, native RGPD compliance, HDS anticipation.
Key figure: +55% cyber attacks on French healthcare establishments by 2024.
A single data leak = lethal for a startup. CNIL sanctions up to 4% of worldwide sales. Loss of trust. Impossible HDS certification.
Our framework :
- EBIOS RM health risk analysis
- Secure architecture from MVP (HDS J1 hosting, AES-256 encryption, strong authentication)
- Operational RGPD compliance (treatment register, PIA, DPO)
- Tested incident response plan
Gain: No post-launch migration. Integrated security = savings of €150-300K.
Pillar 4: Open technical interoperability
The catch: “We’ll make the connectors if the customers ask for them.”
The approach: Interoperability right from the MVP stage, open standards (FHIR), prioritized connector strategy.
The reality: Healthcare establishments use 50-150 different software packages. Your solution needs to integrate, not work in silos.
Example of failure: brilliant AI tool for clinical decision support. But forced doctors to manually re-enter 15 fields already in the DPI. 4 minutes/patient × 30 consultations = 2 hours lost/day. Adoption < 5%. Project abandoned.
Pillar 5: User-centered business design
The trap: “We’ve made a beautiful interface, users will adapt.”
The approach: Co-design with end-users, business UX adapted to field constraints.
Health UX specificities: frequent interruptions (every 4 min), high cognitive stress, heterogeneous digital skills, safety imperative (UX error = serious clinical consequence).
Methodology :
- Field observations (immersion services)
- Iterative co-design (wireframes tested with 8+ real users before coding)
- Permanent User Committee
- Non-negotiable UX principles (efficiency, safety, adaptability)
Success indicator: SUS > 75/100, adoption > 70% at 3 months post-deployment.
Pillar 6: AI and ethical data science
The catch: “We train our algorithm on open source data, that’s enough.”
The approach: responsible AI, clinical explicability, rigorous validation, ethical governance.
Why is this? Healthcare AI is not consumer AI. A diagnostic algorithm that gets it wrong = potentially fatal medical error, medico-legal liability, impact on trust in the healthcare system.
Real case: Readmission prediction algorithm developed on data from Paris University Hospital. Excellent test performance (AUC 0.89). Rural UHC deployment: poor performance (AUC 0.62). Population bias not detected. Delay 8 months.
Framework IA responsible :
- Multidisciplinary ethics committee (doctors, data scientists, lawyers, patients, ethicist)
- Formalized IA ethics charter
- Data representativeness analysis (bias prevention)
- Explicability implemented (SHAP, LIME)
- Mandatory prospective clinical study
- Ongoing post-deployment monitoring
Case study: from 0 to 3 UHC customers in 18 months
Startup: Remote monitoring solution for heart failure patients
Initial stage: Pre-seed, technical prototype, 0 customers
Objective: CE marking + 3 pilot university hospitals in 18 months
Month 1-2: Audit reveals
- Unclear regulatory classification
- No user validation
- Non-HDS cloud architecture
- Algorithm trained on non-representative US dataset
Structuring results :
- Classification IIa confirmed, prospective clinical study planned
- Pivot identified: targets = coordinating nurses (not doctors)
- HDS host migration, full RGPD compliance
- Easily DPI connector (70% French university hospitals)
- Co-design with 8 nurses: SUS 58 → 82/100
- Re-training algorithm French cohort 2400 patients
At 18 months :
- CE marking obtained (on time)
- 3 pilot hospitals signed up (240 patients remotely monitored)
- Clinical study: -34% rehospitalization vs. control
- Seed round €1.2M (vs. €600K expected)
- Publication European Journal of Heart Failure
Key success factor: User pivot identified Month 2. Without structuring, discovery Month 12+ = critical loss of time/money.
5 fatal mistakes to avoid
Error 1: False technological priority
“We’re developing our revolutionary AI for 18 months, then we’ll look at the regulations.”
→ Regulatory compliance IS the limiting factor.
Error 2: “We know better than the users” syndrome
“Our team understands the problem, no need for interviews.”
→ 80% of founding hypotheses are invalidated by the field.
Error 3: Cosmetic safety
“We’ll put in HTTPS and a password for the MVP.”
→ A security flaw instantly destroys trust.
Error 4: The digital island
“We’ll make the connectors if the customers ask for them.”
→ A solution that doesn’t fit in will never be adopted.
Error 5: Black-box AI
“Our algorithm works very well, no need to explain how.”
→ Clinicians will never adopt an AI they don’t understand.
Evaluate your project: JuliaShift matrix
Where do you stand on each of the 6 pillars (scale 0-5)?
| Pillar | Score |
|---|---|
| 1. Regulatory | ___ /5 |
| 2. Go-to-Market | ___ /5 |
| 3. Security | ___ /5 |
| 4. Interoperability | ___ /5 |
| 5. UX design | ___ /5 |
| 6. Ethical AI | ___ /5 |
| TOTAL | ___ /30 |
Interpretation :
- 0-10/30: High-risk project → Recasting necessary
- 11-18/30: Fragile foundations → Structuring 2-3 critical pillars
- 19-24/30: Good trajectory → Strengthening before scaling
- 25-30/30: Excellence → Maintain continuous improvement
Why this methodology works
Data on 30 supported projects (2023-2025) :
- Success rate: 73% market reach (vs. 30% industry average)
- Time-to-market: 35% reduction (regulatory anticipation, no late recasting)
- Fundraising: Average amounts +40% (structured projects = investor confidence)
- User adoption: +45% (systematic co-design)
- ROI on structuring: 12x on average (investment €85K → premium of €1M)
Successful projects are not the most technically brilliant. They are the most methodologically rigorous.
Your next steps
- Diagnose your situation: 6-pillar assessment matrix + identification of 3 priority risks + recommended 90-day roadmap.
- Talk to us: Express project maturity analysis, identification of bottlenecks, customized recommendations.
- Structure your project
To find out more
- CNIL – RGPD and health data
- HL7 FHIR – Healthcare interoperability
- Bpifrance – France 2030 digital health
Do you have an e-health project to structure?
Let’s talk about your context. Maturity diagnosis, identification of critical risks, structuring roadmap.
👉 Book free discovery audit 30 min
🎯 Going further
Are you structuring a MedTech fundraiser?
Download our free strategic reports:
- BPI France 50-point compliance checklist
- Timeline 0-6 months pre-emergence
- 3 startup cases (seed → series A)
- Frameworks valorisation multiples Revenue
📥 Download your free reports → Blueprint MedTech
About the author
Nicolas Schneider is a strategic consultant in digital healthcare transformation and founder of JuliaShift. With 17 years’ experience at the Service de Santé des Armées and 8 years in digital transformation consulting, he assists MedTech startups and healthcare establishments in their financing strategy, structuring pharma partnerships and preparing for fund-raising.
Specialties: healthcare innovation financing, MedTech fund-raising structuring, pharma industrial partnerships, IA regulatory compliance.